
Rheumatoid arthritis vs. lupus: What’s the difference?

When it comes to autoimmune diseases, rheumatoid arthritis (RA) and lupus are often mentioned. They share certain characteristics, but they are distinct conditions with unique symptoms, causes and treatments. Understanding these differences is crucial for effective management and treatment. This article explores various aspects of both rheumatoid arthritis and lupus, helping you to identify and differentiate between them.
What is rheumatoid arthritis?
Rheumatoid arthritis is a chronic inflammatory disorder that primarily affects joints. It occurs when your immune system mistakenly attacks your body's tissues. Unlike the wear-and-tear damage of other types of arthritis, rheumatoid arthritis affects the lining of your joints, causing a painful swelling that can eventually result in bone erosion and joint deformity.
What causes rheumatoid arthritis?
The exact cause of rheumatoid arthritis is not fully understood, but it is known that genetics, environmental factors and hormones might contribute to its development. Certain genes can make you more susceptible to environmental factors, such as infections with certain viruses and bacteria, that may trigger the disease.
Signs of rheumatoid arthritis
Common symptoms of rheumatoid arthritis include tender, warm, swollen joints; joint stiffness that is usually worse in the morning and after inactivity; fatigue; fever and a loss of appetite. Symptoms may vary in severity and can come and go.
What is lupus?
Lupus, or systemic lupus erythematosus (SLE), is a chronic autoimmune disease that can cause inflammation and pain in any part of your body. It’s an unpredictable disease that can affect the skin, joints, kidneys, brain and other organs.
What causes lupus?
The exact cause of lupus is unknown, but it is believed to result from a combination of genetics, environment and hormones. Certain factors, such as sunlight, infections and medications, might trigger symptoms in people who are susceptible to lupus.
Signs of lupus
Lupus symptoms can mimic other health issues, making it difficult to diagnose. Common signs include fatigue, joint pain, swelling, headaches, a butterfly-shaped rash on the cheeks and nose, hair loss, anemia and blood-clotting problems. Like rheumatoid arthritis, symptoms of lupus can vary over time.
Key differences between rheumatoid arthritis and lupus
While both rheumatoid arthritis and lupus are autoimmune diseases with overlapping symptoms, there are significant differences between the two.
Affected areas
Rheumatoid arthritis primarily targets the joints, although it can also affect the skin, eyes, lungs and heart. Lupus, however, is more systemic and can attack any part of the body, including the skin, joints, kidneys, brain and other organs.
Nature of symptoms
Rheumatoid arthritis often results in consistent pain and swelling in the joints, while lupus symptoms tend to be more sporadic, often appearing and disappearing without a predictable pattern.
Diagnosis
Diagnosing rheumatoid arthritis often involves blood tests that look for specific markers, such as rheumatoid factor or anti-citrullinated protein antibody (ACPA), as well as imaging tests like X-rays. Lupus diagnosis is more challenging and typically requires a combination of blood tests, urine tests and physical examinations to identify the presence of autoantibodies and evaluate symptoms.
Treatment approaches
The treatment approaches for rheumatoid arthritis and lupus differ significantly because they target different aspects of the immune response.
Early diagnosing and treating both rheumatoid arthritis and lupus is vital in order to prevent long-term outcomes or damage to the body. Fortunately, there has been significant advances in diagnostic tests and treatments for both conditions.—Sharon Barnhart, NP, Gundersen Rheumatology
Treatment for rheumatoid arthritis
Treatments for rheumatoid arthritis focus on managing symptoms and preventing joint damage. Common medications involved include NSAIDs (nonsteroidal anti-inflammatory drugs), corticosteroids, DMARDs (disease-modifying antirheumatic drugs) and biologics.
Treatment for lupus
Lupus treatment aims to manage symptoms and prevent flare-ups. It often involves NSAIDs, antimalarial drugs, corticosteroids and immunosuppressants. Each patient’s treatment plan is unique and can change over time based on how the disease progresses.
Pain relief strategies
Both diseases require effective pain management strategies to improve quality of life.
Arthritis pain relief
For arthritis, pain relief often involves medication, physical therapy and lifestyle changes. Regular exercise, weight control and stress management are essential components. Some patients find relief with hot and cold therapies, acupuncture or massage.
Lupus pain relief
Lupus pain relief may include medications, such as NSAIDs or corticosteroids, and lifestyle modifications like a balanced diet, regular exercise and stress reduction. Avoiding sunlight and using sunscreen is critical for those with lupus to prevent skin-related symptoms.
Living with rheumatoid arthritis and lupus
Living with either condition requires a comprehensive management plan and regular communication with your healthcare providers. For more information and how to get connected with a Gundersen Rheumatology provider, call 608-775-1395 or visit Rheumatology | Gundersen Health System. Both diseases can affect mental health, so support from family, friends and professional counselors is important. Joining support groups can also provide emotional assistance and valuable information.
Understanding the differences between rheumatoid arthritis and lupus is crucial for effective management and treatment. While they share some similarities as autoimmune diseases, their differences in symptoms, causes and treatment approaches are significant.
By staying informed and proactive in managing your health, you can lead a fulfilling life despite the challenges posed by rheumatoid arthritis or lupus. Remember, early diagnosis and treatment can significantly improve outcomes and enhance your quality of life.
If you suspect you have symptoms of either condition, talk to your primary care provider about the next steps in getting an accurate diagnosis and appropriate treatment plan.
Related articles

Exploring the benefits of red light therapy

LASIK eye surgery: Is it right for me?
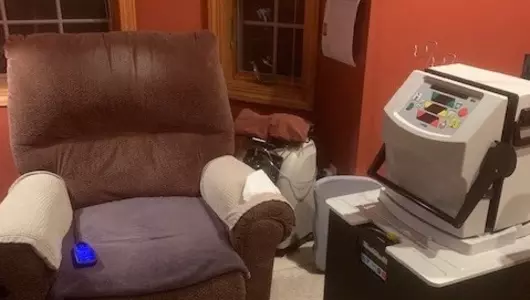
Empower your health: The freedom of home dialysis over in-center hemodialysis

Lip blushing is the key to fuller lips – without the fillers